Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mario Brondani*1 and Adriana RB Siqueira2
Received: November 07, 2017; Published: November 14, 2017
Corresponding author: Mario Brondani, Associate Professor, Director, Dental Public Health Graduate Program, Department of Oral Health Sciences, Division of Preventive & Community Dentistry, and Prosthodontics and Dental Geriatrics, University of British Columbia, 2199 Wes brook Mall. Vancouver, BC, V6T 1Z3, USA
DOI: 10.26717/BJSTR.2017.01.000527
Objective: This paper aims to present a generalized farm-to-fork surveillance system framework with a focus on education for improving health and controlling and preventing food borne illnesses.
Method: A brief literature search compiled some of the existing surveillance systems with special attention to the Canadian context. The Public Health Agency of Canada conceptual model for food borne surveillance was used to develop a framework focused on educating the public on controlling and preventing food borne illnesses.
Result: The farm-to-fork surveillance system presented focuses on the end-user as well as producers and food handlers, with special attention on how to keep illness-causing pathogens out of food, destroy them once they have contaminated the food, and control their growth in already contaminated food. There are many local and worldwide efforts on how to properly hand-sanitize before, during and after food preparation in restaurants/eateries and at home so that food borne illnesses are prevented.
Conclusion: A food borne illness surveillance system is needed in Canada focusing on introducing a harmonious and standardized surveillance system across the country; strengthening local and provincial capacity for implementing such surveillance and in responding to food borne illnesses through networking; and enhancing the surveillance capacity along the entire farm-to-fork chain.
Food borne illnesses result from consuming contaminated food or beverage with infections (bacteria, viruses, parasites, and prions) and non-infectious (poisonings - fungi and their toxins, heavy metals, chemical, and so on) contaminants at any stage from farm-to-fork chain [1,2] Every year in the U.S.A, food borne illnesses cost more than US$150 billion in medical expenses and economy loss due to days of work missed; cause 5000 fatalities and more than 76 million reports of illness-related symptoms. It is believed that one in every six Americans (or 48 million people) gets sick with foodborne diseases from 31 known pathogens annually [3] Between 1990 and 2004, there were 639 outbreak reports linked to contaminated produce in the US, including those related to tomatoes with Salmonella served in restaurants, and lettuce with E. coli O157: H7 served at the Taco Bell© fast food chain. In Canada, readyto- eat meat products contaminated with Listeria monocytogenes resulted in 57 confirmed illnesses and 22 deaths across the country in 2011 [4] In order to respond faster, more efficiently and more effectively to national and international foodborne outbreaks, the Food-borne Illness Outbreak Response Protocol (FIORP) was updated by the Public Health Agency of Canada in 2010 [5] After the FIORP updated, there were at least four outbreaks in 2016 and 2015, two involving Salmonella infection, one involving Listeria from packaged salad products from the Dole processing plant in Springfield, Ohio and another involving Vibrio para haemo lyticus linked to raw shellfish [6].
Contaminated foods commonly associated with food borne illness are [7].
a. Animal in origin (beef, poultry, eggs, milk, soft cheese, seafood, and so on);
b. Raw fruits and vegetables;
c. Canned products (canned goods, juices, cider, and so on).
Since 2009, the Government of Canada offers an annual food recall report which, for the first six months of 2011, for example, this report showed seven recalls on products contaminated with E. coli O157: H7, 18 recalls on products contaminated with Listeria, 23 recalls on products contaminated with Salmonella, just to namea few [8]. Although American and Canadian data might be alarming, food borne illnesses are still underreported locally and worldwide, and go undiagnosed as people fail to come forward about all food poisonings and do not always seek a doctor when feeling ill. When people seek care, the medical system fails to issue a specific diagnosis [9]. Once the source of contamination is identified following a report, food recall occurs. In general, public companies affected by a recalled product can experience share price volatility, and have their stock price dropping 30% within the first week of recalls.
In 2009 the Kellogg’s© lost nearly $70 million worth of peanut butter crackers and cookies recalled contaminated with Salmonella [10] In 2017, Thomas concluded that on average, an initial recall involving meat and poultry products for example, is associated with short-term reductions in shareholder wealth of up to $236 million, 5 days after the recall announcement [11] The primary sources of pathogens found in foods are from a variety of sources: feces (intestinal tracks of animals and humans), soil and water, plants and plant products, food equipment and utensils, animal feeds, animal hides, food handlers, processing plant air and dust, and more. With such a variety of contact points in which food can get contaminated, people are both the main cause and the victims in food borne illnesses. Once contaminated foods are ingested, people can be highly contagious before any symptoms appear and even after symptoms disappear. Hence, about half of healthy food handlers are carriers of disease agents. Improper handling and sanitation in food preparation (in restaurants and other eateries, and at home) are critical to preventing food borne illnesses and yet, many people do not know how to properly do it. As a result, educating the public about food safety (handling, storage and preparation) is the outcome focus of the surveillance system presented in this paper for use in a public health action to reduce morbidity and mortality and to improve health [12].
Surveillance is ‘the ongoing and systematic collection, analysis, interpretation, and dissemination of data about health-related event for use in a public health action to reduce morbidity and mortality and to improve health [13] and it is necessary to determine any significant change in frequency (outbreaks) and distribution of cases [14]. Although food borne illnesses are underreported, there are various worldwide surveillance systems in place aimed at interrupting the transmission of food-related pathogens [9,15,16]. Unfortunately, ‘the need for a Canadian food and nutrition surveillance system has been recognized for some time’ despite of the existence of a conceptual model on surveillance proposed by Health Canada [17] and its FIORP [5]. Hence, there is an inconsistency on how and what to report, which adds difficulties in comparing the different surveillance systems despite the existence of guidelines [11] and worksheets [9].
Based on the different foodborne illnesses surveillance systems available [12,18] the following framework is suggested (Figure 1). A suggested food borne illness surveillance system involving data collection, analysis, dissemination and application (Figure 1) highlights four main components of a surveillance system: data collection (who, when, what and where – case definition), analysis (what food and contaminants are implicated, and the need for laboratory confirmation), dissemination (to health authorities and the public), and application (the means used to prevent further spread, and can include education, food recalls, inspections and regulations).The art in surveillance lies in collecting appropriate and timely information and in interpreting it correctly, which might lead to controlling the outbreak [9]. Upon analysis of all the information gathered, a suspicion of a foodborne illness case can be raised and the local health authority notified (either from thehealth care provider, laboratory, or other source) (Figure 1). The public is then made aware of the potential outbreak, and food recall occurs. Despite the effort, however, food borne illnesses remain under reported because, for each case that gets identified through clinical laboratory analysis, another 29 are estimated to go unreported [19]. Moreover, them is understanding of the food handling or consumption, changes in consumption patterns due to food shortages, mass food recalls and regulatory changes in food safety can only make food borne illness surveillance fallible [10,20].
Figure 1: A suggested food borne illness surveillance system involving data collection, analysis, dissemination and application.
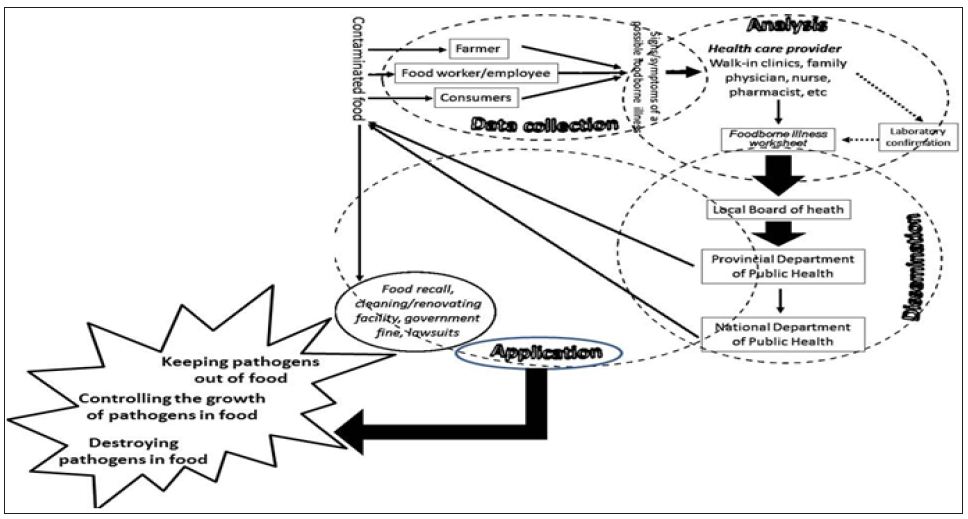
The success of the application aspect of a surveillance system has to go beyond food recalls, government fines, and lawsuits to include public education on how to prevent the contamination and spread of food borne illnesses. This education involves the preparation and dissemination of information on food safety to the public at large. Information can be provided to advise the public on: how to keep illness-causing pathogens out of food, how to destroy illness-causing pathogens or how to control their growth once they have contaminated the food, as follows:
Information should focus on building sanitary barriers between food handlers/consumers and the foodthey manipulate/eat and educate them on how to proper handle food. The ‘Food-Safe School Action Guide’ in the [21] US educates school children and staff on washing produces under running water; removing and discarding outer leaves from lettuce and cabbage; washing hands before preparing food, when switching from one type or food handling to another, and after preparing food; and regularly cleaning and disinfecting the refrigerator, freezer, and counters. The guide does reinforce hand-washing as the single most important method of preventing food contamination [22,23]. In fact, the United Nations has declared the 15th of October as the Global Hand-washing Day to improve hygiene practices worldwide. In order to avoid food contamination by employees, many public eateries have a reminder in their washrooms advising their employers about a step-by-step process on how to properly wash and dry all areas of their hands before returning to the kitchen or counter area. In New Zealand, campaigns are more direct with respect to the consequences of poor hand-washing by mentioning diarrhoea and vomiting.
These campaigns have been emphasizing that there is no need to use an antibacterial soap to do a good job and hand sanitizers should not replace of plain soap and water. However, the WHO recently suggested alcohol-based handrubs as the best option to fulfill the highest standards of safety in relation to the prevention of cross-infection when focusing on point of care [24] alcoholbased handrubs have to yet be proven efficacious and safe in handling food and food products. At the farm level as well as in commercial food operations and distribution plants, best practice guidelines on food production and handling should include inspection of fields and packing plants; utilization of third party audits to monitor workers’ hygiene; testing dairy, meat, and food products for microbial contamination regularly; inspect plant after an outbreak; coordinate food recalls carried out by industry; and so on. Health agencies have regular food handling inspections for food establishments, and food handlers must have a valid Food Safe BC certificate to ensure that proper food handling procedures are observed and practiced in British Columbia, Canada [25]. It is noted that despite these efforts, there is no guarantee that proper food handling procedures are followed accordingly.
The main focus here is in eliminating pathogens that have already contaminated food during production, storage or preparation. Such destruction can takes place via thermal processing (mainly cooking-heat temperature at recommended levels accordingly for different foods); non-thermal processing (irradiation, pulsed electric fields, oscillating magnetic fields, high pressure processing, pulse light technology, and freezing at commercial level); antimicrobial and sanitizers (ozone, chlorine, iodine, and organic acids at commercial level); or hurdle technology (combine interventions methods to prevent bacterial growth at commercial level). The Canadian Food Inspection Agency has an online document alerting the population about the proper way to cook meat and poultry products while other online resources offer food storage guidelines for cupboard, refrigerator and freezer [26,27], in various languages such as Dari, Cambodian and Zulu [28]. The ‘Food-Safe School Action Guide’ [15] reinforces cooking time and temperatures, and the importance in maintaining heat in hot foods; separation of raw meat from cooked foods and vegetables including cleaning cutting boards that contacted raw meat; chilling food by refrigerating leftovers promptly and at right temperature; keeping purchased (refrigerated) food chilled until getting home; and reheating leftovers properly.
Bacterial growth is a major source for food borne illnesses either from raw, uncooked, and improperly cooked food, or from not appropriately stored cooked food. Although there are various factors affecting bacterial growth (type of food, acidity of food, time and temperature, oxygen and moisture), the existing guidelines reinforce the need for refrigerating foods at 40o Fahrenheit (about 4.4o Celsius) or lower within two hours or less after cooking, and not leaving standing water in sinks. The World Health Organization has developed the ‘five keys to safer food’ campaign [28] that is available in more than 50 languages and reinforces the above points as well as the need to remind consumers and eateries to not thaw frozen food at room temperature, but in the fridge. Hence, getting information from government websites [5] and from numerous web pages including ‘Livestrong’ [29] and online blogs might further help to reinforce food safety practices. Food blogs such as the ‘food buglady’ [30] offers updated lists of food safety recalls in Canada, while the ‘Gainesville’s Lunch out Blog’ [31] discusses issues of contamination in the U.S fast food chains. Despite the efforts outlined above, a foodborne outbreak can still happen, and it remains up to those affected individual to seek medical attention to disseminate information, which can be used to identify or warn others of potential contaminations. For example, in 2007, participants from a muddy BC cross-country mountain bike race commented on a race-related web forum that they were feeling ill with similar symptoms. Such internet activity prompted the race organizers to contact the local public health unit, which then received 13 laboratory reports of Campylobacter jejuni outbreak infection in the racers who ingested mud [32].
Aside from the variation of food contaminants and case definition, the underreported status of food borne illnesses, the lack of a firm Canadian surveillance system, other barriers exist in making the public aware of food borne illness. For example, there are unanswered questions about the influences of the social, cultural and physical environments in which the social aspects of food consumption and eating behaviour occur [33] including:
a. How do advertising and the mass media affect the nutritional knowledge and perceptions of Canadians?
b. What is the relationship between socio-cultural and economic status and diet?
c. What are the interactions between the individual and collective determinants of healthy eating that are unique to older adults?
d. How are the dietary habits of Aboriginal people influenced by concerns over pollutants in their local food sources?
e. What impact do self-esteem and body image have on food selection and eating behavior?
f. Another barrier regards to the perception of food borne illness risk. The lay perspective of health risk is personal and differs markedly from the expert view which tends to focus on a more impartial point of view in regards to food hazards [34]. The public’s perceptions are important to be considered by health agencies when tailoring information on how to minimize the risks and public health burden of food borne illness, and on how to promote confidence in the food chain supply.
Another limitation happens in terms of food recall. According to Maple Leaf Foods, many Canadian small markets do not have a food recall plan to readily identify the immediate previous supplier and the immediate subsequent recipient of food in case of an outbreak [35]. Larger companies such as Safeway Inc, Loblaw Companies Limited, Save-on-Foods© and Costco Wholesale Corporation use personalized membership or loyalty cards to offer discounts to their loyal customers. These companies can trace purchases through the loyalty cards, which can assist in identifying purchasers of a recalled product and promptly inform the consumers.
A national food borne illness surveillance system focusing on educating the public at large is needed to monitor patterns of diseases that occur within the farm-to-fork chain. Such education should include proper hand sanitation, food storage and food preparation since the globalization of the food supply also brings the globalization of food borne illnesses. In Canada, a food borne illness [36] surveillance system could be modeled on the framework presented in (Figure 1), focusing on [28]:
a. Introducing a harmonic and standardized surveillance system across the country;
b. Strengthening local and provincial capacity for implementing such surveillance and in responding to food borne illnesses through networking; and
c. Enhancing the surveillance capacity along the entire farm-to-fork chain.
In addition, careful attention has to be placed on the eating habits of a multicultural and multi-language society such as that in Canada and in British Columbia while encouraging the public to engage more proactively in coming forward and reporting their food borne illness symptoms to a health provider/authority. The authors would like to caution the readers that (Figure 1) has not been tested or evaluated.
This manuscript was produced as part of the requirements for a graduated course called ‘Introduction to Public Health Surveillance’, under a Master in Public Health degree via the University of British Columbia School of Public and Population Health by the first author in 2012. The authors are grateful to the course instructor, Dr. Svetlana Kishchenko, for her insightful guidance and ideas. The authors also acknowledge Mr. Glenn Knowles for his comments and suggestions on the style of the paper.


