Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Fabio G F*
Received: November 01, 2017; Published: November 10, 2017
Corresponding author: Fabio Gonçalves Ferreira, Liver and Portal Hypertension Group, Surgery Department, Santa Casa de Sao Paulo School of Medical Sciences, Sao Paulo, Brazil
DOI: 10.26717/BJSTR.2017.01.000514
Huge hepatocellular carcinoma (>10cm) resection it is not frequent in cirrhotic livers due to high mortality rates and poor survival rates. Nevertheless, patients with normal livers have a different prognosis, and can bear until 80% liver resection. This case reports the 60-year-old female patient with abdominal tumor and big in the records of any liver disease. HCC diagnosis was achieved with imaging exams and high blood levels of Alpha-fetoprotein (AFP). Surgical removal was proposed, the left trissegmentectomy. This case shows radical tumor resection the curative treatment.
Key words: Hepatic Neoplasia; Hepatocellular Carcinoma; Hepatectomy; Trissegmentectomy; Hepatic Node
Abbreviations: HCC: Hepatocellular Carcinoma; USG: Ultra Sono Graphy; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; HCC: Hepato Cellular Carcinoma; TACE: Trans Arterial Chemoembolization; AFP: Alpha-Feto Protein
Hepatocellular carcinoma (HCC) is the primary malignant tumor of the liver, being the fifth most frequent malignant tumor and the third in terms of mortality. Its incidence is estimated to be between 500,000 to 1 million cases a year and is more frequent in tropical countries, underdeveloped or developing. It is more common in males, between the ages of 50 and 60 years, with the ratio of 8:1 in high incidence regions and ranging from 1.5 to 3:1 in regions of low incidence. Its etiology is directly linked to cirrhosis of the liver, as well as to infection by hepatitis virus’s B and C, alcohol consumption, aflatoxin contamination and metabolic diseases, liver being the most important hemochromatosis. HCC has variable clinical presentations, depending on the presence of cirrhosis, typically, degree of tumor liver failure or atypical manifestations and, being more findings Paraneoplastic frequent: weight loss, hepatomegaly, abdominal pain, ascites, jaundice, fever and splenomegaly [1,2]. Laboratory changes arising from the HCC are non-specific and depend on the tumor extension and severity of liver injury. AFP high above 400mg/mL makes the diagnosis; however, 20 to 30% of cases may have normal AFP. Imaging research methods are essential for the diagnosis of the HCC, with the most employees the ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI).
The treatment can be divided into curative: partial resection, liver transplantation, ablative therapies or palliation: TACE, hormone therapy, chemo/radiotherapy, symptomatic and supportive treatment. Despite the cirrhosis is one of the most important risk factors for the development of the HCC, approximately 10 to 15% of cases the liver is normal. Patients without a history of chronic liver disease are rarely diagnosed early, usually are not conducted routine tests for these patients (USG abdomen or dosage of AFP), then the diagnosis is made late, when the patient exhibits symptoms due to large tumor mass. In these cases there is no transplant indication according to the criteria of Milan (single tumor less than or equal to 5 cm, or no more than 3 tumors smaller than 3cm) and non-surgical therapies such as trans arterial chemoembolization (TACE), percutaneous radiofrequency ablation, percutaneous ethanol injection and microwave coagulation therapy have been shown to be ineffective. The only curative treatment in these cases would be resection by more than 60% of patients [3,4].
Female patient, 60 years sought the emergency room of Santa Casa de Misericordia de Sao Paulo hospital complaining of abdominal pain and vomiting for 2 months. Pain was diffused throughout the abdominal region accompanied by weight loss of 10kg in 2 months. Concerns have noticed increased abdominal volume, jaundice accompanied by pruritus. Patient was bleached +/4+, her history revealed jaundice +/4+. Flaccid abdomen, painful mass in right hypochondrium palpable until umbilical scar. CT scan (Figure 1) revealed large expansive mass with lobulated margins on the anterior surface of the liver, which featured the heterogeneouscontrast enhancement. Such lesion measured about 17.6 x 18.4 x 14.3 cm, occupied all the left lobe and part of the right lobe of the liver. Also enhanced numerous small vessels within the lesion. There was also other smaller satellite lesions. Gallbladder with homogeneous content and small diffuse parietal thickening. Bile duct dilatation most evident in the left lobe. Small amount of free fluid in pelvic cavity, presence of splenomegaly and aortoiliac iliac atheromatous plaques. In laboratory tests showed increased liver enzymes: alkaline phosphatase of 2231U/L (70-290 U/L), gamma glutamyl transferase of 989U/L (< 38 U/L), TGO of 307U/L (8-33 U/L), TGP of 114 (7-35 U/L), AFP greater than 1000ng/ml (up to 8ng/ml), bilirubin total 12.8mg/dL (0.3-1.2mg/dL), direct bilirubin of 7.4mg/dL (0.3-1.2mg/dL) and indirect bilirubin of 5.4mg/dL (up to 1.0mg/dL).
Figure 1: CT scan showing a large expansive mass with lobulated margins on the anterior surface of the liver and heterogeneous contrast enhancement measuring 17.6 x 18.4 x 14.3cm.

There was then the diagnosis of HCC and surgical treatmentleft trissegmentectomy was proposed. In the inventory of the cavity (Figure 2) was able to see right lobe of the liver of habitual aspect and a tumor of approximately 30cm in diameter in the left lobe, rejecting the whole liver and gall to right side, without diaphragm without implant adhesions peritoneal and without evidence of thrombosis of the portal vein. There was difficulty to access the bifurcation of Portal vein because large tumor growth, being necessary to perform first dissection of hepatic veins with bandage and the left and face liver diaphragmatic detachment. Resection was performed at all left lobe the bloody area covered with biological glue. Hilar lymphadenectomy was performed. In intra operative was necessary to 4units of blood transfusion and infusion of vasoactive drugs. The anatomical and pathological report showed surgical piece (Figure 3) the left lobe, caudate lobe and square lobe weighing and measuring 3052g 21x20x11cm. The cuts had greenish tumor, rounded contours and well delimited by measuring hepatic parenchyma in the adjacent 17x11cm displaying 3 nodes of 0.9 to 3cm of diameter 0.5 to 1cm distant from the lesion and with the same characteristics. It was observed the presence of necrotic foci and microvascular invasion without perineural invasion, surgical resection margin free of neoplasia. All lymph nodes were free of neoplasia. Was observed in trabecular pattern, moderately differentiated (Grade 2) and the pathological staging was T3N0Mx, having confirmation of the diagnosis of Hepatocellular Carcinoma (HCC) by examining- HISTO-Chemistry (positive for antigens: CK7, Hepatocyte and KI67). Patient was transferred to the ICU to vasoactive for 1 day after surgery, where evolved well having high in 2 days to bed in the infirmary, where remained stable, afebrile and without complaints getting high on the 5th day post-op. Currently 22 PO, free of neoplastic disease in outpatient follow-up.
Figure 2: Intraoperative: A) Before resection, B) Final aspect after resection and lymphadenectomy.
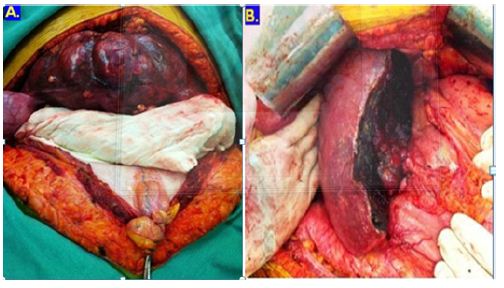
Figure 3: Morphologic aspect and weight (3052gm).

According to the Barcelona criteria, the patient would fit in the C stage, tumor larger than 5cm, multinodular with microscopic vascular invasion. Therapeutic approach proposed by this classification scheme would be palliative treatment with TACE, chemotherapy with Sorafenib or symptomatic treatment and supportive, being contraindicated liver resection [1]. These criteria, however, take into consideration only patients with cirrhosis, in which the resections must not exceed 50% of the liver tissue, unlike patients without chronic liver disease, in which resections can reach 80% [5,6]. Despite the unfavorable prognostic factors that usually accompany the HCC (high rates of AFP, vascular invasion, multipletumors), the size of the tumor itself can be used as a parameter for contraindication of resection [7]. Lang et al. [3] compared survival among 1, 3 and 5 years in patients with cirrhotic HCC resection, using factors such as: the presence of hepatitis B and C, the presence of fibrosis, resection greater or less than 50%, multifocal, or tumor size greater than 5 cm , degree of differentiation, TNM classification, among others. Framing the patient in this study, we would observe the following survival rates at 1, 3 and 5 years respectively: patients suffering from viral hepatitis 79, 51 and 35%; without fibrosis, 79, 54, 36%; resection more than 50%, 68, 39, 20%; multifocal tumor, 72, 42, 21%; size greater than 5 cm, 74, 48, 29%; moderately differentiated tumor, 70, 32, 18%; TNM stage IIIA, 65, 39, 29% [4].
In a systematic review conducted by Zhou Y-M et al in 2011, survival rates were observed in 1, 3 and 5 years of 60.7, 34 and 28.6% in patients undergoing resection with tumors larger than 10cm. The study considered the partial hepatectomy as therapeutic method considerably me assist in these patients compared to non-surgical options [8]. Although the patient present 17x11cm tumor, not presented macroscopic vascular invasion, cirrhosis, viral hepatitis, low degree of differentiation or capsular invasion, which represent important factors of poor prognosis, opting for the curative resection. Although the only potential treatments represent dressing for these patients, there are still very few studies concerning the effectiveness of partial liver resection in relation to other therapeutic methods. Data indicate that survival rates in noncirrhotic patients undergoing hepatectomy range from 46 to 76% in 3 years and 26 to 68% in 5 years. Data on disease-free survival are scarce, but suggest rates ranging from 24 to 56% in 5 years [3]. The recurrence of the HCC can result from new development of tumor by underlying disease or metastatic dissemination. In patients with cirrhosis, it is more common for recurrence metastasis of hematogenous dissemination. This indicates that even a more aggressive approach as the total hepatectomy would not be enough to prevent relapse [3,4].


