Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Paredes Ingrid MD1, Herrera Gonzalez Aaron MD*2, Venkataraman Priyanka MD3, Winn Heather MD4 and Anasti James MD2
Received: October 23, 2017; Published: October 30, 2017
Corresponding author: Aaron Joel Herrera Gonzalez, 801 Ostrum St, Bethlehem, PA 18015, ORCID: 0000-0001-7724-4044
DOI: 10.26717/BJSTR.2017.01.000474
The Effect of 6 Weeks versus 3 Weeks Post Partum Visit on Short Interval Delivery Rate.
Objective: To evaluate the effect of postpartum visit timing on short interval delivery rates.
Methods: Retrospective chart review was conducted on all patients who had two deliveries at a large community hospital resident’s clinic between May of 2011 to January 2013. Patient demographics, breast feeding, economic status, and postpartum visit attendance were compared to patients that had only one delivery during that time period. From May 2015 to January 2017, 18 months after altering the timing of postpartum visit from 6 to 3 weeks, the short interval delivery and attendance at postpartum visit were compared between the two time periods at the same clinic. Univariate analysis using Chi square or t -test were used as appropriate.
Results: During the initial study phase 72 (7.3%) out of 991 patients had a short interval delivery. Only age (25.4 ± 6.4, 27.9 ± 5.1, p=0.001) and attendance at the postpartum visit (49.6% vs. 63.6, p=0.02) differed between the short interval delivery and the non-short interval delivery groups. In the follow up period (May 2015 to January 2017), 53 (5%) out of 1056 deliveries were short interval deliveries. Postpartum visit attendance was 752 (71.2%). Significant decrease in short interval pregnancy was noted when comparing the two time periods (7.3% vs. 5%, p=0.04). In addition an increase in PPV attendance was noted (62.1% vs. 71.2%, p=0.001).
Conclusion: Changing the timing of the postpartum visit from 6 weeks to 3 weeks may decrease short interval delivery rate and increase postpartum visit attendance.
Keywords: Short; Interval; Delivery; Pregnancy; Postpartum; Visit
The World Health Organization recommends ideal pregnancy spacing between 18 and 60 months [1]. In the United States the recommended interval between pregnancies has not yet reached a consensus. However, in the literature, short interval pregnancy (SIP) has been defined between 6 and 18 months from live birth to conception of a subsequent pregnancy [2]. SIP has been associated with multiple maternal and neonatal complications. Preterm premature rupture of membranes, preterm birth, placental abruption, congenital anomalies, low birth weight, autism, schizophrenia, fetal and maternal death have all been noted to increase with SIP [3].
Interestingly, in the United States, risk factors for SIP include college education, childbearing after 30 yrs of age, and private insurance benefits [2]. This indicates a group that may have a wish for a SIP. From the literature, those that have a SIP of less than 6 months are at the highest risk of poor pregnancy outcomes and as such may benefit most from intervention [4]. It has been reported that SIP (less than 6 months) is more common in lower social economic groups, younger ages, lower educational levels and in those receiving suboptimal prenatal care [5,6]. The National Survey of Family Growth, reports that in the United States, unintended pregnancy rates are as high as 50% with a third of them meeting criteria for SIP [2].
The economic burden of these unintended pregnancies is estimated at 11billion dollars per year [7]. The postpartum period or puerperium, defined as the time between the delivery of theplacenta and generally considered to end six weeks postpartum, is critical for the prevention of SIP. Immediate initiation of postpartum contraception at the postpartum visit (PPV) is the intervention that has had the greatest impact in reducing SIP [8]. The convention of the six week PPV is based on older non evidence based expert opinion [9]. Most women resume sexual activity before 6 weeks after delivery and, in the non-breastfeeding woman, ovulation can happen as early as 25 days postpartum [10]. Interestingly, many providers counsel their patients to schedule their postpartum visit 6 weeks after delivery, thus loosing valuable time for the timely initiation of birth control. We chose to use two deliveries in an 18 months time frame as short interval deliveries. Based on this information we hypothesized that women with short interval delivery (SID) would be more likely to miss their postpartum visit (PPV). Furthermore, techniques to increase attendance at the PPV would in turn decrease SID. The following study was designed to answer these questions.
Charts were reviewed of all patients that had 2 deliveries during an 18 month period (May 2011 to January 2013) from a residency clinic at a community hospital. The study was approved by St. Luke’s institutional review board. The short interval deliveries (SID) were compared to patients who only had one delivery during this time period (non-SID). We compared the following variables; age, parity, employment status, insurance coverage, race, breastfeeding, attendance at postpartum visit (PPV) and Depo-Provera post delivery all related to first pregnancy. Separate univariant analyses on the above variables were performed comparing SID to non-SID patients. The information obtained from this analysis was used to develop a protocol to apply prospectively to our clinic population to decrease SID. In a follow up time period, May 2015 to January 2017, we compared SID to the above previous study period. The proportion of SID as well as the percentage of all patients that attended their PPV was compared to the previous time period. Chi square and t- test were used as appropriate. A p value of 0.05 or less was considered significant. Correction for multiple measurements was not performed. Statistical calculations were done utilizing Sigma Stat software (Systat Software, San Jose, CA)
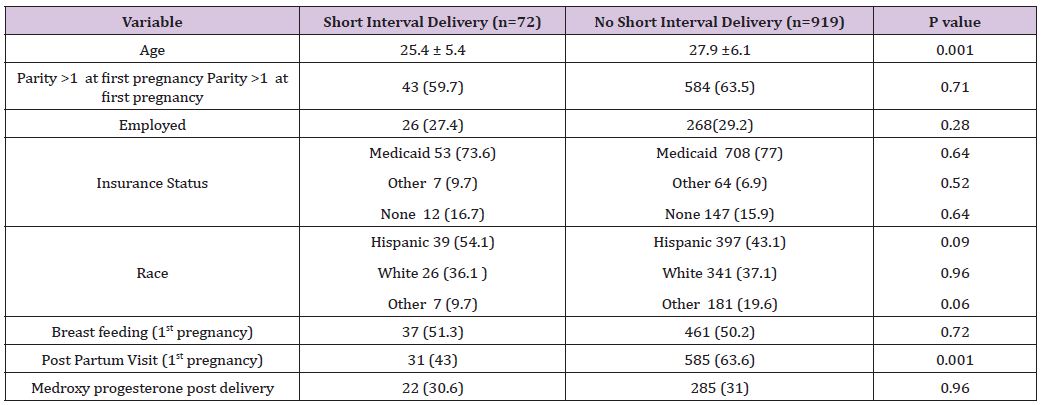
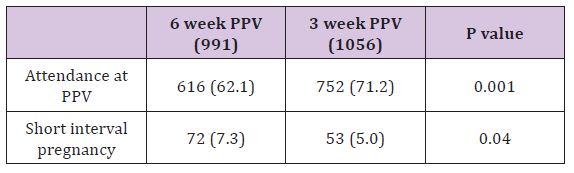
During the initial study phase 991 deliveries were performed, of which 72 (7.3%) were SID. PPV attendance was 616 (62.1%). Only younger age (25.4 ± 6.4, 27.9 ± 5.1, p=0.001) and attendance at the PPV (43.1% vs. 63.6, p=0.02) differed between the SID and the non SID group (Table 1). The only modifiable variable was attendance at the PPV. Based on these finding, a PPV program was developed that included moving the PPV from 6 weeks to 3 weeks in attempt to increase PPV attendance. In the follow up period of the 1056 deliveries, 53 (5%) were SID and PPV attendance was 71.2% (n=752). Significant decrease in SID was noted when comparing the two time periods (7.3% vs. 5%, p=0.04). In addition an increase in PPV attendance was noted (62.1% vs. 71.2%, p=0.001).
Table 1: Comparison of Characteristics of Short Interval Delivery to Non -Short Interval Delivery during Initial Phase of Study.
We noted that a younger age and failure to attend their PPV after first pregnancy were increased in SID as compared to non-SID in our population. From this information, we altered the timing of the PPV from traditional 6 weeks to 3 weeks, in an attempt to increase PPV attendance. In the second phase of our study we noted, an increase in our PPV attendance and a decrease in SID. Thus, suggesting a 3 week PPV as a possible intervention to decreasing SID. Previous studies have shown that the initiating of contraception in the postpartum period is an effective tool in decreasing SIP [11]. National data has demonstrated that up to 40 % of patients fail to attend their postpartum visit [12]. Novel approaches to increase PPV attendance can provide a timely venue to discuss and prescribe contraception. This in turn will decrease the SIP. Another approach to increase prenatal care is the offering of incentives, such as coupons, cash, and merchandise. Although some of these studies noted an increase in attendance at prenatal care visits, they were no more likely to return for a PPV than the non- incentivized controls [13]. Furthermore, short interval pregnancy was not an outcome measure in these incentivizingstudies. We chose to use two deliveries in an 18 months time frame. We employed these criteria for several reasons. It was a definable end point that could be obtained from our current databases (Table 2).
Table 2: Comparison of Attendance of Postpartum Visit (PPV) at First Pregnancy and Short Interval Delivery (SID) Between Phase 1 (6 Week PPV) and Phase 2 (3 Week PPV) of Study.
Trying to determine if an individual had a positive pregnancy test or a termination after a live birth was fraught with validity difficulties. Lastly, this endpoint of 2 deliveries in 18 months may identify the greatest risk group for potential pregnancy complications and hence the appropriate subset of SIP that would benefit from an intervention [1]. Although we have noted no adverse clinical outcomes since altering the timing of our PPVs, our study was underpowered to look at improvement in detection or failure to identify problems as a result of altering PPV timing. The 6 week PPV is based on the physiology to allow for sufficient time for involution of pregnancy. This timing of the PPV is based on no discernable evidence [14]. The traditional timing of PPV may relate to a time when less effective contraception was available. Studies have shown that between 20 and 60% of women has had intercourse by 6 weeks postpartum [15]. The return of ovulation can occur as early as 26 days postpartum and 78% of women have ovulated before their “first post partum” menses [16]. For these reason, the starting of contraception prior to 6 weeks seems prudent.
Although we encourage long acting reversible contraception (LARC) in appropriate individuals, estrogen containing contraception was also prescribed at the 3 week PPV. These medications were avoided in breast feeding patients and in those that may be at higher risk of venous thrombosis. This includes obesity, smokers, difficulty in ambulation and other medical complications. If these individuals were not amenable to other forms of birth control, then combined contraception was started after 6 weeks. There are several strengths of our study. It was performed on a stable population that is not transient. Although minor deviation from individualizations can occur, major counseling, treatments, and follow up are protocol driven, ensuring evidence proven standard of care. We chose two time periods to allow for adequate implementation of our revised PPV protocol and decreasing the chance of overlapping study participants. As noted earlier, we defined our SIP as two deliveries in the dedicated time periods. This ensured validity in our measurements and also identified those pregnancies at highest risk for poor outcomes. Lastly, during the both study phases the only immediate postpartum contraception available was medroxy progesterone.
This eliminates the bias of immediate postpartum LARC on the incidence of SID. There are some noted weaknesses to our study. A randomized study design would have allowed for a more effective method to control potential biases that may occur over time. Although our definition of SIP has its value, it could be considered a weakness, because it fails to identify a large population that maybe at risk for subtle outcome concerns. The time period was considerable for this project. Thus, different clinician and changes in patient population may have occurred. The difference we found in attendance at PPV and decrease in SID were statistically significant in our two cohorts, but our study was underpowered to analyze more clinically important outcomes, such as preterm labor, preeclampsia, LBW, or other morbidities. SIP can lead to poor pregnancy outcomes. Postpartum contraception is a proven intervention that has decreased SIP rate. However, to implement postpartum contraception novel approaches are needed to ensure the patient can receive it. Changing the PPV from the standard 6 to 3 weeks may be one technique to provide clinician-patient interaction to educated and prescript postpartum contraception in a timely fashion.


