Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Syed Kamran Ali Shah1*, Syed Shahid Noor2, Mehroze Zameer3, Kazim Rahim Najjad4 and Asad Khan Ghilzai5
Received: October 19, 2017; Published: October 25, 2017
Corresponding author: Syed Kamran Ali Shah, Dept. of Orthopaedics, K-Block, Liaquat, National Hospital, Stadium road, Karachi, Pakistan
DOI: 10.26717/BJSTR.2017.01.000465
Objective: To determine the effectiveness of no drain placement compared to use of closed suction drain post TKA, in terms of wound related complications and blood loss.
Methods: This prospective observational study was conducted at Liaquat National Hospital, Karachi, from April 2016 to March 2017. Clinical data including co-morbidities, pre operative haemoglobin and indication for TKA were collected in the Performa. All patients randomized into even and odd number sub divided into Group A (without post operative drain) and Group B (with closed suction drains). Tourniquet were applied in all cases, after completion of TKA tourniquet were released and bleeding points controlled. Group B patients were received closed suction drains followed by wound closure, whereas Group A patients undergo direct closure without drain placement. Pre operative haemoglobin were collected and repeated on 1st and 5th postoperative day. At 5th postoperative day dressing were changed and wound assessed for any wound related complications and total number of blood transfusions required also noted. Data were collected manually and analysed using SPSS version 19.
Result: Out of 120 enrolled patients, 28(23.33%) were male and 92 (76.66%) females, overall mean age (62.92±8.73). In group A 41 (68.33%) patients experienced wound edema in comparison to group B which had 7(11.66%) patients with wound edema. Mean haemoglobin drop pre and post operatively on 5th day were 2.000±0.972 mg/dl in group A compared to group B 2.713±1.042 mg/dl. Haemoglobin drop among two groups were significant, Mean total number of blood transfusion required in group A were 1.53 ±0.833 pints in compared to group B which were 2.48 ±0.676 pints and found statistically significant.
Conclusion: Without use of drain have drastically decrease the rate of transfusion and perhaps the transfusions related complications which includes cross match and hypersensitivity reactions and also the transfer of blood born diseases which can be lethal to life. But contrary there were some wound related complications which can be addressed by homeostasis and meticulous wound closure.
Keywords : Knee Arthroplasty, Drainage, Hemoglobin, Complications
Total knee arthroplasty (TKA) is a major orthopaedic procedure carried out in mostly elderly population. It is a very frequently performed surgery but it’s not without the risk of bleeding and infection. Sehat et al. [1] observed that mean blood loss in TKA can range up to 1474 ml. The use of post operative drainage in TKA patients has been the topic of debate for many years and still there is no clear guidelines established in the literature. Reilly et al. [2] found that placement of drainage tube in TKA results in more blood loss than without drainage tube whereas Fan Y et al. [3] has discouraged the placement of drain as it may lead to an increased risk of retrograde infection. Moreover post operative drain usage in TKA is associated with an astounding increase in cost of over $400 per knee in a recent study [4]. Al-Zahid [5] in his study on over a hundred TKAs found no significant difference in terms of wound complications, blood loss and functional outcome. A Polish study also favored not to use drains post operatively as authors noticed lesser number of dressing change during hospitalization and also lower need of opioid analgesia [6].
No studies have been conducted in Pakistan for TKA patients regarding drainage in the post operative period. We wish to evaluate our population in a randomized controlled trial on this aspect and hopefully to establish a local guideline for efficient, cost effective and safe management of TKA patients. The aim of our study to evaluate the difference between two groups of drain verses no drain placement in total knee replacement patients with respect to wound related complications, level of hemoglobin dropped post operatively and units of blood transfused post operatively. Our aim was also to establish a local guideline for efficient, cost effective and safe management in total knee arthroplasty patients.
This was a prospective observational study conducted at the Department of Orthopaedic Surgery, Liaquat National Hospital and Medical College, Karachi. April 2016 to March 2017. Patients were registered using a predesigned Performa. Approval from institutional ethical review committee was taken prior to commencement of the study. Formal informed written consent was obtained from patients registering in the study. Using a nonprobability, consecutive sampling technique 120 patients were registered for the study.
a. Inclusion Criteria
i. Either gender
ii. Patient in age limit 50-85 years
iii. Bilateral knee osteoarthritis or rheumatoid arthritis requiring bilateral TKA
b. Exclusion Criteria
i. Patients on anticoagulant therapy or with clotting disorders
ii. Patients with renal or hepatic function impairment
iii. Revision or complex primary knees requiring extensive tissue dissection
After meeting the inclusion and exclusion criteria, patients were included in the study. Specific clinical data including the co-morbidities, pre operative hemoglobin of the patient and indication for TKA were collected in the Performa that is provided in the study tool section. Patients were sub divided into Group A (N=60) (without post operative drain) and Group B (N=60) (with closed suction drains). All patients undergo bilateral TKA by single surgeon. Tourniquet applied in all cases and leg elevated before inflation of tourniquet. In all the patients, simultaneously bilateral posterior-stabilized TKA was carried while using midline incision with medial par patellar approach. All the patients included in the study received standard tibial and femoral implant. Patellar resurfacing was done in all patients.
After completion of implantation of prosthesis tourniquet was released and bleeding points were controlled prior to closure. After control of bleeding group B patients received size 14 drainage tubes connected to a closed suction bottle followed by wound closure, whereas group A patients were undergo direct closure without drain placement. Hemoglobin levels were repeated at 1st and 5th postoperative day and noted in the Performa. At 5th postoperative day dressing were changed and wound complications such as blister formation, wound edema, superficial marginal skin necrosis, superficial wound dehiscence and local superficial infection were checked. Also total number of blood transfusions required were monitored and recorded in the Performa. Comparison of mean hemoglobin values at 1st and 5th postoperative day, number of units of blood transfused were calculated using Independent t test taking P<0.05 as significant. Associations of different wound related complications with group A and group B were demonstrated by using Chi square test taking P<0.05 as significant (Figure 1).
Figure 1 : Representing frequency of wound related complications between two groups.
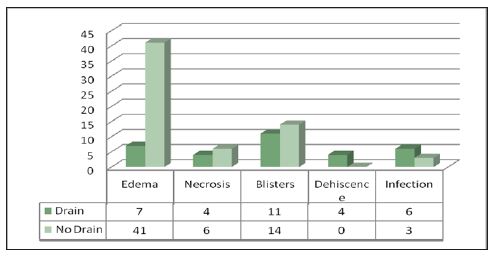
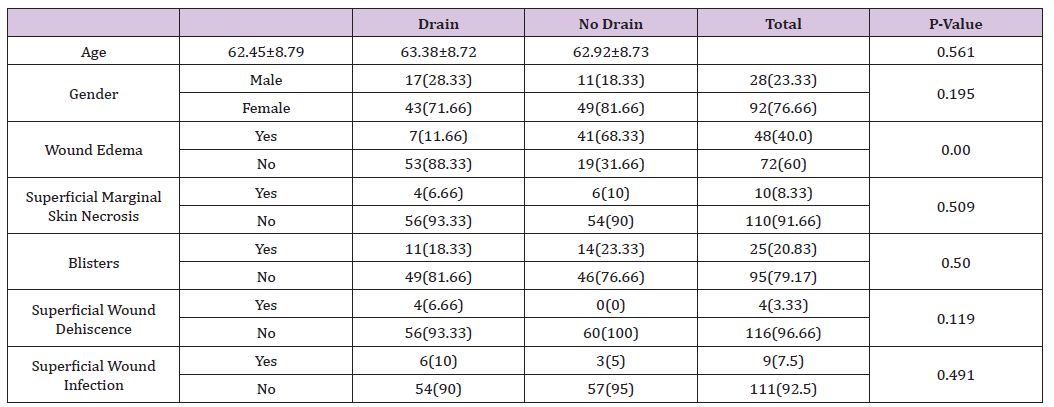
Out of 120 enrolled patients, 28(23.33%) were male and 92(76.66%) females, in which group A 11(18.33%) were male and 49(81.66%) patients were female and in group B 17(28.33%) male and 43 (71.66%) female patients. Mean age in group A is 63.38±8.72 years and in group B mean age is 62.45±8.79, overall mean age 62.92±8.73. In group A (No Drain) 41(68.33%) patient’s developed wound edema while in group B only 7(11.66%) patients experienced wound edema. Superficial marginal skin necrosis was seen in 6(10%) patients of group A and in group B 4(6.66%) patients experienced. 14(23.33%) patients in group A developed Blister and in group B 11(18.33%) patients experienced blister formation (Figures 2 & 3).
Figure 2 : Showing Mean of Pre and Post OP Haemoglobin.
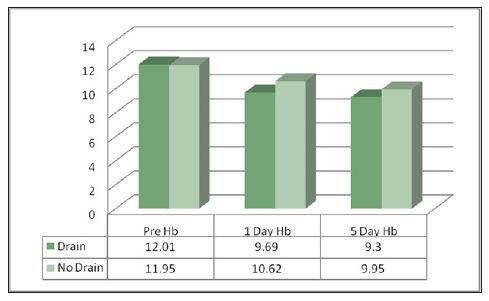
Figure 3 : Showing Mean of required number of transfusion between two groups.
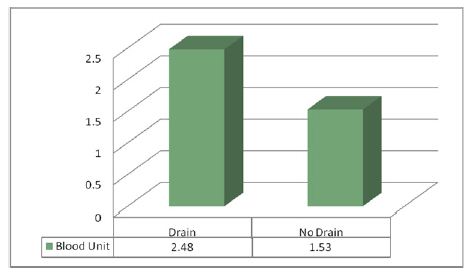
None of the patients in group A developed wound dehiscence comparison to group B in which 4(6.66%) patients suffered from wound dehiscence.6(10%) patients in group B represents local wound infection postoperatively comparison to group A in which 3(5%) had wound infections. Pre operative mean hemoglobin levels of group A were 11.952±0.9454 mg/dl and their mean hemoglobin drop post operatively were on 5th day 2.000±0.972 mg/dl in compared to group B mean pre op hemoglobin levels were 12.017±0.929 mg/dl and their post operative mean hemoglobin drop were on 5th day 2.713±1.042mg/dl. Hemoglobin dropped among two groups was significant. Mean total units of blood transfused in group A were 1.53±0.833 in compared to group B 2.48±0.676 (Tables 1 & 2).
Table 1 : Distribution of patients with respect to age, gender and wound related Complication between two groups.
Figures are in mean ± SD. Independent t-test was used for comparative analysis statistically significant p-value < 0.05
Table 2 : Shows mean of pre op haemoglobin, haemoglobin differences and required no transfusion among two groups.
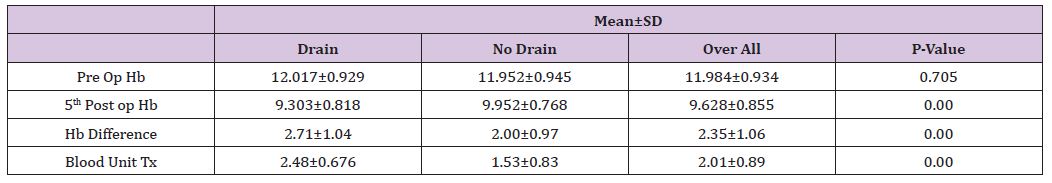
Figures are in mean ± SD. Independent t-test was used for comparative analysis statistically significant p-value < 0.05
Uses of drainage in total knee arthroplasty patient are to prevent hematoma accumulation, to decrease the risk of infection, and to minimize complications and adverse events. Controversy still surrounds the use of drains after total knee arthroplasty. In United Kingdom a survey was conducted for all members of the British Orthopedic Association, which showed that 94% of surgeons accounting for 80% of all total knee arthroplasty, was using closed suction drainage, due to fear of increase risk of infections and hematoma formation [7]. Fan Y et al. [3] has discouraged the placement of drain as it may lead to an increased risk of retrograde infection. Holt favored the use of drains in terms of less need of dressings during the early post operative period and decreased incidence of ecchymosis and wound complications [8].
In comparison to above mentioned studies, in our study we noticed no statistical difference observed for wound related complications like skin necrosis, blister formation, wound dehiscence and wound infection in total knee arthroplasty among these groups, except we noticed 41 patients developed edema, in non drainage group, and it was significant comparison to drain placement group. In this study our 6 patients developed superficial wound infection in drainage group and 3 patients in no drain placement group but statistically no significant difference found among two groups. A retrospective study conducted by Demirkale et al. [9] revealed that decreased rate of wound infection and minimal needs for blood transfusion observed in non-drainage group of total knee arthroplasty. Another study in which Passad studied the risk factors associated with greater blood loss and need for blood transfusion [10]. They stated that a significant correlation between tourniquet time and operation duration. Pavone et al. [11,12] explained the need for blood transfusion in patients undergoing one-stage bilateral knee replacement.
Higher blood loss will be expected in patients with use of suction drain [13]. Mengal et al. [14] concluded that no difference in post-operative Hb levels but higher rates of blood transfusion were required in the no drain group. Kumar et al. [15], Sundaram and Parkinson [16] both failed to show a statistically significant difference between the two groups using post-operative Hb levels and autologous transfusion rates as outcomes. Demirkale and other above mention author’s studies had positive association with our study as we noticed decreased needs for blood transfusion and hemoglobin difference in no drain placement group was statistically significant, which also reduces the risk of transfusion related complication .We confirm these results since we noticed significant hemoglobin drop post operatively in drain placement group with increased number of transfusion comparison to without drain placement group. The possible explanation of this is that the presence of a drain reduces the tamponade effect. The strength of our study based on the minimization of confounding variables. The patients in this single surgeon series were recruited over a short time and post-operative care was identical in all cases.
Without use of drain have drastically decrease the rate of transfusion and perhaps the transfusions related complications which includes cross match and hypersensitivity reactions and also the transfer of blood born diseases which can be lethal to life. But contrary there were some wound related complications which can be addressed by homeostasis and meticulous wound closure. It was a single centre prospective study value.


